Treatment : Multi-disciplinary approach (Doctors)
The Role and Function of Primary Care Physician in Diabetes Care
Diabetes is a growing problem
The World Health Organization (WHO) estimates that the number of persons who have diabetes may double to 300 million by the year 2025, of which 90–95% will be type 2 diabetes.1,2 The National Health and Morbidity Survey 2011 showed that diabetes affect about 2.5 million people in Malaysia.3 It is the leading cause of morbidity and mortality.4,5
For most of us in primary care, diabetes is among the main condition we handle in our practices – but how certain are you that you are caring optimally for your patients with diabetes? The national audit data in 2009 reveal a wide gap between guideline recommendations and the care that patients’ receive.6
Broadly defined, intensive diabetes management aims to achieve optimum glycaemic control using advanced techniques i.e oral anti-diabetic agent, insulin therapy, self-monitoring of blood glucose (SMBG), nutrition, and behavioral changes.7 Intensive management is far more than increased frequency of monitoring or an additional injection of insulin per day. It requires careful follow-up to monitor progress toward individualized goals and support to reinforce management skills and personal efforts.
Such complexities extend beyond the scope of solo practitioners. It is not surprising that intensive diabetes management requires a core-group of skilled professionals with diverse roles, functions, and contributions : the interdisciplinary team.
The interdisciplinary, integrated care team as a model for the treatment of chronic illness is not a new concept. Its benefits have been supported in a variety of disorders.8-10 Adoption of this model is relatively new to diabetes, however, and requires a shift in how diabetes providers view their roles and relationships, both with patients and with professionals in other disciplines.
How Can The Quality of Management Be Improved?
This can be done by focusing on primary prevention by :
- encouraging lifestyle changes among patients at risk such as those with metabolic syndrome and obesity.
- screening populations at high-risk; and
- clinical diabetes management, as encouraged by the Clinical Practice Guideline (CPG) Management of Type 2 diabetes mellitus.7
It would be helpful to identify individuals with diabetes and be more aggressive about setting and tracking haemoglobin A1c, lipid and blood pressure progress towards goals. It would also be nice to put into practice a recall system when the patient with poorly controlled diabetes and hypertension default their clinic appointments. It is really important to discuss behavioural modifications to which the patients can commit, given the ample time and resources required to care for this chronic disease.11
Diabetes should be moved from an after thought to the main course. Many interventions have been shown to improve outcomes in diabetes mellitus. Education measures work; and they include performing chart audits, giving reminder cards, pharmacist collaboration, using flow sheet, and certain nursing initiatives. 12
What is Team Management?
Composition of the Diabetes Treatment Team
The interdisciplinary, integrated diabetes treatment team includes primary care physicians, physicians/endocrinologists, assistant medical officers, nurses, and dietitians.13 This core membership reflects the basic requirements of diabetes treatment : nutrition, medication, self-monitoring, and self-management. Team skills are designed to address the regular, recurring needs of most people with diabetes.
Teams may also extend to health care professionals who can help meet special or specific needs not within the scope of the core team’s expertise. For example, pharmacists, exercise physiologists, ophthalmologists, podiatrists, or specialists in maternal-child care or gerontology may have a place within the diabetes care team.
The existence of a diabetes care team implies the development of a comprehensive diabetes care program ensuring that standards of care are met.13 Care should be research-based and outcome-focused. Mutual support of team members will encourage on-going professional development and support of critical thinking skills.7,14
In the team management of diabetes the patient is the central member. For patients to accept responsibility for self-care they must understand the condition, its effect on health and the practicalities of management. Good communication between team members is important so that advice is consistent and not confusing for the patient.
The following professionals are important in the team approach to diabetes:7
Primary Care Physician
The primary care physician has the central role in coordinating management of the person with diabetes and in education, counseling and softening the “technology/person interface” often felt by people with a chronic condition. The primary care physician is the point of first contact and usually will be responsible for the overall management. In some instance where a diabetes educator or a dietitian is not available the primary care physician and/or the clinic nurse must carry out the comprehensive education for the patient.
Diabetes Educator
The diabetes educator can often spend more time than the primary care physician has available, consolidating the patient’s knowledge and skills regarding eating plan, physical activity, self-monitoring, medication usage, foot care etc.
Dietitian
The role of the dietitian in the management of diabetes is paramount. Lifestyle changes alone (healthy food and regular exercise with ensuing weight loss) are sufficient for glycaemic control in the majority of patients with newly diagnosed type 2 diabetes. Recommendations should be individualized to maximize cooperation. Early referral to a dietitian is desirable to ensure detailed education on this most important aspect of management. The primary care physician must understand the principles of dietary advice to be able to reinforce the dietary recommendations for the patient.3
Endocrinologist / Diabetologist / Paediatrician
The advice of a specialist physician may be valuable for people with complicated problems related to diabetes – especially children, adolescents and adults with type 1 diabetes or diabetes in pregnancy. A shared care approach by primary care physician and specialist will provide the best combination of specialized expertise and continuity of care. In many cases the specialist will be part of an organised, multi-disciplinary diabetes care team which can provide a comprehensive diabetes education program.
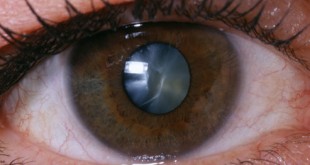
Ophthalmologist / Optometrist
All people with diabetes need to have vision test and eye assessment done regularly in the primary care set-up. Early detection of retinopathy, before visual loss occurs, markedly improves prognosis for sight. Certain retinopathy changes or deterioration in vision requires referral to the ophthalmologist.
Oral Health Professional
Dental and periodontal problems are common in people with diabetes who need to see a dentist regularly (e.g: yearly).
Podiatrist
The podiatrist renders expert preventive care. If there is evidence of neuropathy, micro- or macro-vascular disease or anatomical problems with the feet, early referral is desirable and regular review is necessary.
Exercise professional
When initiating a physical activity program in a patient who has been relatively inactive, the help of a physiotherapist with a special interest in exercise routines or an exercise physiologist may be beneficial.
Role and function of Primary Care Physician
Family physicians can contribute to the country’s diabetes prevention efforts by implementing the steps listed in the table.
| Table 1. Patient-Centered Function of a Diabetes Care Team |
· Educate about the disease process. · Promote problem-solving skills. · Identify resources to promote self-care. · Develop short- and long-term diabetes care goals. · Prescribe and implement plan for achieving goals. · Medication. · Exercise. · Diet. · Behavioural modification. · Screen for diabetes complications. · Identify risk-factors. · Refer to appropriate specialists.
|
Now that diabetes experts agree that metabolic control matters, early diagnosis of diabetes with aggressive treatment designed to achieve and maintain near-normal blood glucose control is imperative. Achieving these goals requires a better approach to diabetes treatment.
On-going treatment of diabetes by a multi-disciplinary team is feasible and facilitates the achievement of treatment goals that will result in the development of fewer long-term diabetic complications.
References
- King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care 1998; 21: 1414–31.
- Cockram CS. The epidemiology of diabetes mellitus in the Asia-Pacific region. Hong Kong Med. J. 2000; 6: 43–52.
- Malaysian National Health Morbidity Survey 2011. Ministry of Health
- Stamler J, Vaccaro O, Neaton JD, et al. Diabetes, Other Risk Factors, and 12-yr Cardiovascular Mortality for Men Screened in the Multiple Risk Factor Intervention Trial. Diabetes Care 1993; 16: 434 – 444.
- Stratton IM, Adler AI, Neil HA, et al. Association of Glycaemia with Macrovascular and Microvascular Complications of Type 2 Diabetes (UKPDS 35): Prospective Observational Study. Br Med J 2000; 321: 405 – 412.
- Mastura, I, Chew, B, Lee, P et al. Control and Treatment Profiles of 70,889 Adult Type 2 Diabetes Mellitus Patients in Malaysia – A Cross Sectional Survey in 2009. International Journal of Collaborative Research on Internal Medicine & Public Health 2011; 3:98-113
- Ministry of Health. Clinical Practice Guideline Management of Type 2 Diabetes. 2009
- Vinicor F: Interdisciplinary and intersectoral approach: a challenge for integrated care. Patient Educ Counsel 26:267-72, 1995
- Stephan F, van Eeden. A multidisciplinary approach to the treatment and management of chronic obstructive pulmonary disease. BCMJ, Vol. 50, No. 3, April 2008: 143-147
- Hart MK, Millard MW. Approaches to chronic disease management for asthma and chronic obstructive pulmonary disease: strategies through the continuum of care. Proc (Bayl Univ Med Cent). 2010 July; 23(3): 223–229.
- Bodenheimer T, Lorig K, Holman H, Grumbach K: Patient self-management of chronic disease in primary care. JAMA 288:2469-2475, 2002
- Grauw WJ et al. Outcomes of audit-enhanced monitoring of patients with type 2 diabetes. J Fam Pract. 2002 May;51(5):459-64.
- McGill M, Felton AM. New global recommendations: A multidisciplinary approach to improving outcomes in diabetes. Primary Care Diabetes. 2007. Vol 1 (1):49-55.
- Top of Form Bottom of F14. American Diabetes Association: Standards of medical care for patients with diabetes mellitus. Diabetes Care 21 (Suppl. 1):S5-12, 1998.
- Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA: The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med 17: 243-252, 2002.
- Anderson RM: The team approach to diabetes: an idea whose time has come. Occupational Health Nurs 30:13-14; 66, 1982.
 PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia
PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia