Why is it important?
Prevention of infection is of paramount importance to solid organ transplant recipients who are immunocompromised, meaning they have reduced immunity due to the transplant medication they are required to take.
Infection in these patients results in a very high risk of illness and death, and treatment with antibiotics is often less effective than in patients with normal immune systems.
The aim of vaccination is to give a person protection (immunity) against specific diseases.
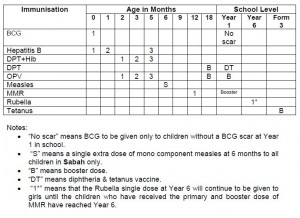
Routine childhood vaccines should be completed according to recommended schedules for the general population before transplantation.
Generally two types of vaccines are used: live attenuated (inactivated) vaccines and inactivated vaccines.
a. Live attenuated (inactivated) vaccines
Consist of tiny quantities of live disease organisms which have been altered so that they cannot cause illness. Our body recognises these weakened organisms and destroys them, and will remember and recognize them to fight them off in the future.
Many immunocompromised patients are unable to produce adequate antibodies after vaccination with live organisms. Furthermore, this may lead to an increased growth of the organisms vaccinated and is therefore generally avoided in solid organ transplant recipients.
b. Inactivated vaccines
Consist of dead disease organisms. Our body recognises these dead organisms and responds to them but in a less vigorous manner compared to live attenuated vaccines.
Patients should wait a minimum of four weeks between live virus vaccine administration and transplantation.
A blood test to determine level of antibodies (ie level of protection against that particular infection ) is recommended prior to transplantation for Hepatitis B and Varicella zoster (chicken pox).
Varicella vaccine
The recommended dose is as follows:
Age 1 -13 years: one dose of varicella vaccine
Adolescents and adults: 2 doses, 4-8 weeks apart
Hepatitis B vaccination
Patients who are going to receive a transplant who have never been vaccinated against the Hepatitis B virus should receive double the recommended vaccine dose immediately, followed by repeat doses after 1, 2 and 6 months. Antibody levels will be checked again 1 month after the last dose.
- Patients who have received the vaccination but have antibody levels less than 100mIU/ml should receive another 3 doses of the vaccine.
- If the antibody level remains negative after revaccination they are not likely to respond to further doses.
Post-Transplant
After undergoing a transplant a patient can ONLY receive inactivated vaccines.
| Vaccine |
Type |
|
Influenza injection |
Inactivated |
|
Hepatitis B |
Inactivated |
|
Hepatitis A |
Inactivated |
|
Pertussis |
Inactivated |
|
Diptheria |
Inactivated |
|
Tetanus |
Inactivated |
|
Polio, inactivated (injection only) |
Inactivated |
|
Haemophilus influenza |
Inactivated |
|
Pneumococcus(conjugated or polysaccharide) |
Inactivated |
|
Neisseria meningitides |
Inactivated |
The following vaccines should NOT be allowed after a transplant:
| Vaccine |
Type |
|
Varicella |
Live attenuated |
|
Measles |
Live attenuated |
|
Rubella |
Live attenuated |
|
BCG |
Live attenuated |
|
Intranasal Influenza |
Live attenuated |
|
Rotavirus |
Live attenuated |
If a person post- transplant is planning on travelling, some vaccines should not be allowed:
| Vaccine |
Type |
Should be allowed post-transplant? |
|
Vibrio cholera |
Inactivated |
Ineffective |
|
Vibrio cholera |
Live attenuated |
No |
|
Yellow fever |
Live attenuated |
No |
|
Japanese encephalitis |
Inactivated |
Yes |
|
Salmonella typhi (injection ) |
Inactivated |
Yes |
|
Salmonella typhi (oral) |
Live attenuated |
No |
|
Neisseria meningitides |
Inactivated |
Yes |
Influenza vaccine
Influenza is a common infection in solid organ transplant recipients and is associated with higher risk of serious illness and death than in others with normal immune systems. In addition to the usual complications of influenza (eg pneumonitis), influenza infection can cause the recipient’s body to reject the transplanted organ.
Routine seasonal administration of the inactivated influenza vaccine is recommended for all transplant candidates and recipients every year, including the first year after transplantation. The intranasal attenuated influenza vaccine is contraindicated in transplant recipients.
Human Papillomavirus (HPV) Vaccine
Transplant recipients are at 20-100-fold increased risk of cancers of the genital tract and high risk for HPV-related warts and skin cancers.
The best time for HPV vaccine is before transplant- at 6 months, 2months and just before transplant in females between the ages of 9 and 26 who are not pregnant.
Summary
- Prevention of infection is of paramount importance to solid organ transplant recipients
- Routine childhood vaccines should be completed according to recommended schedules for the general population before transplantation
- Patients should wait a minimum of four weeks between live virus vaccine administration and transplantation.
- After undergoing a transplant a patient can ONLY receive inactivated vaccines.
References:
- Danzinger-Isakov et al, Guidelines for Vaccination of Solid Organ Transplant, Candidates and Recipients, American Journal of Transplantation 2009; 9 (Suppl 4): S258–S262
- Avery et al, Update on Immunizations in Solid Organ Transplant, Recipients: What Clinicians Need to Know, American Journal of Transplantation 2008; 8: 9–14
- Clinical Practice Guidelines for Renal Replacement Therapy, 4th edition
| Last Reviewed | : | 27 July 2016 |
| Writer | : | Dr. Mirunalini Appadurai |
| Accreditor | : | Dr. Lee Ming Lee |
 PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia
PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia