Introduction
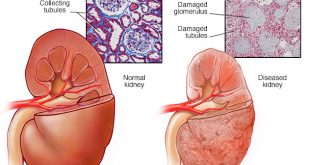
In February 2002, the National Kidney Foundation published clinical care guidelines for chronic kidney disease (CKD). These guidelines help your doctor determine your stage of kidney disease based on the presence of kidney damage and glomerular filtration rate (GFR), which is a measure of your level of kidney function. Your treatment is based on your stage of kidney disease.
|
Stage |
Description |
GFR* (ml/min) |
Action |
|
At increased risk |
Risk factors (e.g., diabetes, high blood pressure, family history, older age, ethnic group) |
90 or above |
Evaluate for CKD |
|
1 |
Kidney damage (e.g., protein in the urine) with normal GFR |
90 or above |
Diagnosis and treatment of other health problems |
|
2 |
Kidney damage with mild decrease in GFR |
60 to 89 |
Estimating progression of CKD |
|
3 |
Moderate decrease in GFR |
30 to 59 |
Evaluating and treating complications (including bone disease) |
|
4 |
Severe reduction in GFR |
15 to 29 |
Preparing for treatment of end stage kidney failure |
|
5 |
End stage kidney failure |
Less than 15 |
Dialysis or kidney transplant needed |
| *, Your GFR number tells your doctor how much kidney function you have. As chronic kidney disease progresses, your GFR number decreases. | |||
Table 1: Stages of CKD and recommended action
People with CKD often develop problems with their bones. It is important to treat bone problems early to keep your bones healthy so you can enjoy better bone health. Sometimes, there are no bone disease symptoms in the early stages of CKD, but without treatment, the bones can become painful and break easily. The heart and blood vessels may also be affected. Your doctor should start checking for bone disease in the early stages of CKD and continue as kidney disease progresses and after you receive your renal replacement therapy (RRT – dialysis or kidney transplant).
Epidemiology
At the end of 2011, the number of people undergoing dialysis exceeded 2 million globally, and in Malaysia there were 25, 688 patients on dialysis (NRR, 2011). Today the global end-stage renal disease (ESRD) patient population continues to grow at an annual rate of 7%, a growth driven by an aging population, increased the incidence of diabetes mellitus and hypertension, improved technology and increased access to treatment. The term, renal bone disease (renal osteodystrophy) is used in a generic sense to include all skeletal disorders that occur in patients with renal failure. The types of bone diseases seen in patients with renal failure are divided into those with accelerated rates of bone turnover (i.e. osteitis fibrosa or hyperparathyroid bone disease and mixed lesions) due to persistently high levels of parathyroid hormone (PTH) and low bone turnover states (i.e., osteomalacia and adynamic lesions) due to aluminium toxicity or relatively low levels of PTH. Some studies showed that high turnover bone disease is the predominant lesion in patients treated with haemodialysis (50 to 60%) whereas low turnover is present in 60 to 70% of patients undergoing peritoneal dialysis.
Causes
Bones are a living and changing part of our body. Old bone layers are constantly being broken down and new bone is being built. Bones are made of cells, fibres, blood vessels, nerves and large amounts of minerals, mostly calcium, and phosphorus. For bones to stay strong and healthy, calcium and phosphorus must stay in balance. Problems arise when these two key minerals get out of balance. This happens with CKD.
CKD affects our bones in three main ways:
- Not enough phosphorus is filtered from blood
Phosphorus is found in most of the foods you eat. When your kidneys are working normally, they filter out excess phosphorus and send it out of the body in the urine. When kidneys are not working properly, phosphorus is not filtered out, and blood levels of phosphorus can become high. This tips the balance between phosphorus and calcium and causes calcium in the blood to become too low. - Too much parathyroid hormone (PTH) is made
Low calcium and high phosphorus signal four small glands in the neck, called the parathyroid glands, to release too much of a hormone called PTH into the blood. The action of PTH is to keep calcium at normal levels by moving calcium out of our bones and into the blood. Over time, more and more calcium leaves the bones, causing bones to become weak and brittle and to break easily. - Vitamin D cannot be activated
When the kidneys are not working well, they can’t take vitamin D from sunlight and food and make it into a type that our body can use (active vitamin D). This also contributes to abnormal levels of calcium, phosphorus and PTH in our blood.

Figure 1: Pathogenesis of High Turnover Bone Disease (Secondary or Renal Hyperparathyroidism) in CKD
Symptoms/Presentations
Bones can be affected as early as Stages 3 and 4 of CKD. Most people do not have any symptoms at these stages of CKD. Even though no symptoms are felt, the bone disease still needs to be treated. Itching may be a sign that phosphorus levels are too high. With more advanced bone disease, other symptoms may appear. This include:
- Bone pain
- Muscle weakness
- Fractures
- Joint pain
Diagnosis
Your doctor will usually order a series of tests and these includes:
- Blood tests: to determine the level of kidney functions, serum calcium, phosphorus, alkaline phosphatase, parathyroid hormone (iPTH) to determine the type and extent of bone disease
- Skeletal x-ray: may be needed to assess the bone involvement



Figure 2: X-ray of skull, hands, and spine
- Bone density scan: a special type of x-ray that measures the thickness and changes in your bones. This test usually examines two areas, the lower spine, and a hip.
- Ultrasound of neck (parathyroid glands): may be needed to assess the size and location of the parathyroid glands
- Bone biopsy: to get a small piece of bone tissue for examination under the microscope. This test may be needed to confirm the diagnosis of bone disease, distinguish the different types of bone disease, guide treatment and provide information about prognosis.

Figure 3: Bone biopsy features of severe high turnover bone disease (osteitis fibrosa)
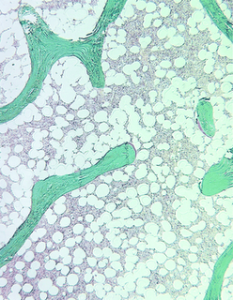
Figure 4: Bone biopsy features of low turnover bone disease (osteomalacia)
Treatment
Steps to maintain bone health may include:
- Controlling your blood phosphorus level by:
- Avoiding a diet that is high in phosphorus.
Dairy Products Vegetables Protein Foods Beverages Other Foods Cheese
Cream soups
Custard
Ice cream
Milk
Pudding
YogurtArtichokes
Asparagus
Brussels sprouts
Dried beans and peas:- Black eyed peas
- Lentils
- Lima beans
- Pinto beans
- Split peas
Organ meats: - Liver
- Kidneys
- Tripe
Oysters
Sardines
Peanut butterAle
Beer
Chocolate milk
Eggnog
Dark colas
Any beverage made with milk or cocoaCaramel
Chocolate
Bean cereal
Brewer’s yeast
Nuts
Seeds
Wheat germ
Whole grain
Quick breads from boxed mixesTable 2: Common High-Phosphorus Foods
- Taking medications called phosphate binders (e.g. calcium carbonate, lanthanum, sevelamer etc.), which bind phosphorus in food while it is still in your stomach. Bound phosphorus cannot get absorbed into your blood and is passed out of your body in the stools when you have a bowel movement. These pills must be taken with your meals and snacks.
- Taking vitamin D compounds, which help to lower your PTH level.
- Exercise
- Exercise can also help to maintain good bone health. The type of exercises that may be helpful are weight-bearing exercises. These include brisk walking, jogging, weight lifting, stair climbing, step aerobics, dancing, racquet sports and others. You should always consult your doctor before beginning an exercise programme.
Patients are also advised to stop smoking, eat healthy a diet and have a healthy lifestyle.
Prognosis /Outcome
Bone disease can develop in the early stages of CKD (CKD III and beyond). However, the types and extent of bone diseases may vary among patients and stages of CKD. Most people do not have any bone symptoms in the early stages of CKD, hence, you should consult your doctor and start checking your calcium, phosphorus, and PTH levels early, and continue when on dialysis or if transplanted. Early management is important to maintain good bone health in CKD.
| Last Reviewed | : | 27 April 2016 |
| Writer | : | Dr. Goh Bak Leong |
| Accreditor | : | Y. Bhg. Dato’ Dr. Rozina Ghazali |
 PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia
PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia