What is asthma action plan?
A written set of instructions plan that tells you what medications to take regularly and how to recognize if your asthma is getting worse, what to do if this happens and how to get help quickly.
How asthma action plan can help you?
Don’t just visit your doctor when your asthma gets worse. Asthma changes over time and by seeing your doctor regularly you can ensure you are taking the right type and amount of medication. Discuss with your doctor on the best and most appropriate treatment.
The plan is designed to tell you what to do when there are changes in the severity of asthma symptoms and in your peak flow readings. It shows you the steps to be taken to prevent your asthma from getting worse. It also provides guidance on when to call your healthcare provider or when to go to the emergency room right away. It also gives you the important health information that can be used in the event of an asthma emergency.
How is asthma action plan designed?
You and your doctor will work together to develop Asthma Action Plan for you. Asthma action plan is personalized to suit individual activities and severity. The plan is designed to tell you what to do when there is a change in the severity of asthma symptoms and in peak flow numbers. This helps you make quick decisions about treatment so that you can avoid more serious attacks and get better.
Your Asthma action plans can be organized in a number of ways. Your asthma action plan may include :
- A list of triggers that are responsible for asthma symptoms and how to avoid them.
- Peak flow meter readings and zones based on the person’s personal-best reading.
- A list of routine asthma symptoms such as coughing, wheezing, chest tightness, shortness of breath, and excess mucus production and what you should do.
- The name and dose of the daily asthma medication that needs to be taken even when you don’t have asthma symptoms.
- The name and dose of the quick-acting or rescue medication that needs to be taken when you develop asthma symptoms.
- The name and dose of the reliever medication that needs to be taken when you are having asthma attack.
- Emergency telephone numbers and locations of emergency care.
- Instructions about when to contact the doctor, whom to call if the doctor is unavailable, and a list of where to get emergency asthma treatment.
Asthma action plan is divided into three zones i.e. green, yellow, and red according to the asthma severity. In each zone, your asthma action plan will give you doctor-written instructions on how to handle each situation.
To determine the zones on your asthma action plan, you have to monitor your own asthma control all the time.
How to monitor your own asthma control?
There are many ways to monitor your asthma control. You can either do your asthma symptoms diary or peak flow rate.
a) Asthma Symptoms Diary
Keeping a diary of your asthma symptoms can help you to identify your triggers. By keeping a record of your symptoms, you can check how well your asthma is controlled, or monitor how your asthma changes over the seasons. Common asthma symptoms include cough, wheeze or chest tightness. Note on your diary the daytime and nighttime symptom and symptoms that occur with activity level (working, exercising or playing).
Example of an asthma diary
|
Date |
Peak Flow Reading/Time
|
Trigger Factors |
Symptoms |
Quick-relief medicine and response | Red zone visit to doctor/
Hospital? |
||
| Green
80% to 100% |
Yellow
50% to 79% |
Red
less than 50% |
|||||
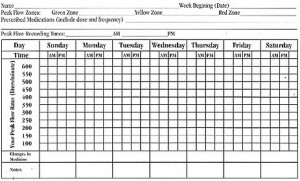
b) Peak Flow Rate
A peak flow test measures how fast you can breathe out. This is also called your PEF: peak expiratory flow. A peak flow meter is the device used to measure how hard and fast you breathe out.
Your doctor will used either your personal best reading or expected value as the benchmark of your asthma control. Your personal best reading is the highest reading you achieve in a two to three week period. Your doctor will calculate your expected peak flow value according to your age, sex and height. Your doctor will use your personal-best peak flow rate to calculate the zones in your asthma action plan.
The peak flow needs to be measured regularly to be useful. Record your scores on a peak flow chart and see how they change over time. Mark on the chart what your score is each morning and evening. You can also mark on the chart when you have taken reliever medication, or things that might affect your asthma. Your peak flow rate can show if your asthma is getting worse, even before you feel symptoms.
If your asthma is not well-controlled your scores are likely to be lower than expected. There also may be a big difference between your morning and evening scores. Talk with your doctor or nurse about what to do when your peak flow changes, or check your Asthma Action Plan.
Peak flow meter
Peak Flow Chart
What you should do?
Take your asthma action plan each time you see your doctor. Your doctor will review your asthma status and adjust your asthma medications, dosages, and frequency, depending on your asthma control (whether green zone, yellow zone, or red zone).
Each time you use your peak flow meter throughout the day, compare the reading with the percentages on your personal asthma action plan. If your peak flow level puts you in the green zone, you’re all clear. If you’re in the yellow zone, read the instructions your doctor wrote down in how to treat the symptoms. If your peak flow level is the red zone, this is an emergency. Read your doctor’s instructions in how to quickly act to reverse symptoms with asthma medication. If there is no change in your asthma symptoms, go to the emergency room or call 911.
Example of Asthma Action Plan
| Date: | Person’s Name / Clinic Number |
| Disease Severity: | |
| Doctor:
Phone: |
|
| Nurse or Therapist:
Phone: |
|
| Evening / Weekend
Phone: |
| Personal-Best Peak Flow (PF):
GREEN ZONE: All Clear ?Where you or your family member should be every day — NO asthma symptoms. Able to do usual activities and sleep without coughing, wheezing, or difficulty in breathing. Peak flow is 80% to 100% of personal best. |
ACTION : Control asthma. Use these medicines every day, on good days and bad days, to prevent asthma symptoms. Use a spacer with metered dose inhalers (or other asthma inhaler and/or medications prescribed for a child).
| Medication
____ |
Dose
____ |
Morning
____ |
Afternoon
____ |
Evening
____ |
Bedtime
____ |
| Medication
____ |
Dose
____ |
Morning
____ |
Afternoon
____ |
Evening
____ |
Bedtime
____ |
| Medication
____ |
Dose
____ |
Morning
____ |
Afternoon
____ |
Evening
____ |
Bedtime
____ |
Use ______ 15 to 20 minutes before exercise or exposure to a known trigger
| YELLOW ZONE : Caution ?This is NOT where you should be. There may be coughing, wheezing, and mild shortness of breath. Sleep and usual activities may be disturbed. You may be more tired than usual. Peak flow is 50% to 80% personal-best. |
ACTION : Relief of Symptoms.
- Keep taking green zone medicines listed above. Use spacer with metered dose inhalers (or
other device prescribed for a child).
- Add quick-relief medicine : _______________ puffs. May use every 4 hours as needed.
Also add : ____________________.
- After taking quick-relief medicine, symptoms should be relieved in 5 to 15 minutes. If symptoms do not improve completely, REPEAT quick-relief medicine 1 to 2 more times, 5 to 20 minutes apart (up to 3 treatments in one hour). (For children, repeat albuterol 1 to 2 more times, 15 to 20 minutes apart; use up to 3 treatments in one hour.) If there is no improvement, call your doctor.
- CALL your doctor or nurse/therapist for further advice.
- If your symptom improves completely after 2 to 3 treatments, continue the quick-relief
medicine 4 times per day for the next 24 hours. Call for further advice.
NOTE : Call the doctor if you or other family member keeps dropping into the yellow zone. The green zone plan may need to be changed to prevent this.
| RED ZONE: Medical Alert — This is an Emergency! ?Red zone means you or your family member, including teenagers and children, need urgent medical care. Symptoms may include frequent, severe cough; severe shortness of breath; wheezing; trouble talking and walking; and rapid breathing. Peak flow is less than 50% of personal best. |
ACTION : Reversal of symptoms
- Take these medicines : Quick relief medicine with spacer ______.
- ADD : __________________.
- If there is no change, GO TO THE EMERGENCY ROOM.
- If you or your family member (including teenagers and children) has trouble walking or talking, is gasping for air, has blue lips or fingernails, or is unable to do a peak flow, this is an emergency. CALL 9-1-1.
- If symptoms improve but do not go away completely, return to the yellow zone plan and
follow the instructions. Call your doctor for further advice.
Note: Always keep your asthma action plan where it can be easily found. Remember to take the asthma diary and asthma action plan to each doctor visit.
| Last Reviewed | : | 16 July 2013 |
| Writer | : | Dr. Jemah bt Sajari |
| Reviewer | Dr. Jamalul Azizi b. Abdul Rahman |
 PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia
PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia