Introduction
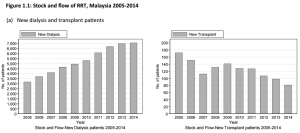
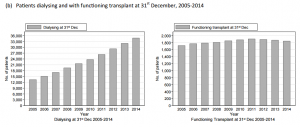
Kidney transplantation is the treatment of choice for end-stage renal disease. The problem is shortage of donated organs and a growing wait list for transplantation. In 2014, there are 34,767 patients on dialysis and the number of new transplant patient for 2014 was only 81.
Who can donate their kidney?
There are 2 types of kidney donation:
- Living donor: the donor is alive and is usually related to the recipient
- Deceased donor:the organs are removed after the donor is pronounced dead (only with family consent)
What is the advantage of living donors?
- Shorter waiting time for dialysis patients compared to waiting for a deceased donor
- Short and long term survival rates are significantly better for transplants from living donors than transplants from deceased donors
- Living donor kidneys almost always start functioning immediately, whereas deceased donor kidneys can take from a few days to a few weeks to start functioning
- The recipient has time to plan for the transplant: procedure is an elective operation
Who can be a living donor?
In Malaysia, the Ministry of Health Malaysia only allows family members (first degree/ second degree relative) or spouse to donate.
| FIRST DEGREE RELATIVE | SECOND DEGREE RELATIVE |
| Parents | Grandparents |
| Siblings | Grandchildren |
| Children | Aunts/ uncles |
| Nephews/nieces | |
| Step siblings |
If you are not related and keen to be a living donor to a dialysis patient, your doctor can apply to the Unrelated Transplant Approval committee (UTAC) for approval. UTAC is an independent committee that was set up by the Ministry of Health Malaysia to evaluate non related living transplant request.
Who cannot be a living donor?
- Children less than 18 years old
- Prisoners
- Individuals with certain health problems:
- Urine protein is persistently >300 mg /day in 3 consecutive samples
- Impaired kidney function
- Hypertension > 140/90 mmHg
- Diabetes mellitus
- Family history of type 2 diabetes mellitus with impaired glucose tolerance test
- Transient gestational diabetes
- Patients with a BMI > 35 kg/m²
- Psychiatric illness e.g. psychotic disorders
- Bleeding disorder
- Systemic illness with potential to develop renal disease
- Active drug abuse e.g. amphetamines, heroin and cocaine
- Severe heart and lung disease
- Infectious disease e.g. HIV and Hepatitis C
- Pregnancy
- Adult polycystic kidney disease
The following are just some of the tests a donor could expect to have during the evaluation process:
- Living donor undergoes a blood test to determine blood type compatibility with the recipient
- Blood group: A, B, O, AB
- HLA Tissue typing: The donor’s blood is drawn for tissue typing of the white blood cells. This test checks the tissue match between six cells of each of the donor and recipient
- HLA cross match:
- A positive cross match means that the recipient has responded that it is likely to reject the donor in which case the transplant should not be carried out.
- A negative cross match means that the recipients’ blood has not reacted to the donor in which case transplantation should be safe.
- Cardiovascular assessment: blood pressure assessment, electrocardiogram (ECG), chest radiography, fasting cholesterol level
- Donor’s kidney function: 24 hour urine sampling for electrolytes/ protein/ creatinine clearance, fasting blood sugar, blood test for renal function and electrolytes, ultrasound kidney, Computer tomography urogram, DTPA renography and renal angiogram
- Assessment of potential risk of transmitting infection to the recipient example hepatitis/ HIV
- Motivation and psychosocial status assessment: The motive to donate to the potential recipient should be entirely altruistic. The potential donor should not be under duress, coerced or induced to donate.
Donors will be evaluated physically and mentally. Risk and complication of all procedures will be explained to potential donors. The doctors in charge of the donor work-up will guard the rights of the potential donor. Potential donor can decide to withdraw donation at any time and their reason will be kept confidential.
Summary
Living donation occurs only when there is informed consent that is freely given. When the procedure is successful the feeling of satisfaction for the donor is a very positive psychological experience knowing that he or she has helped improve the life of a family member in need. There is no way to measure this benefit for the donor but it is very real to the people that experience it.
References
- 22nd Report of the Malaysian Dialysis and Transplant Registry 2014
- Brochure publish by Unit Perkhidmatan Transplan Bahagian Perkembangan Perubatan, Kementerian Kesihatan Malaysia.
- Renal Replacement Therapy Clinical Practice Guideline (MOH) 3rd Edition
- Living Kidney Donor Network Website
| Last Reviewed | : | 17 June 2016 |
| Writer | : | Dr. Shahnaz Shah Firdaus Khan |
| Accreditor | : | Dr. Wong Hin Seng |
 PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia
PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia