Introduction On Insulin Pump
 Figure 1 : An insulin pump model with the home screen showing the reservoir status, time and battery status.
Figure 1 : An insulin pump model with the home screen showing the reservoir status, time and battery status.
An insulin pump (Fig. 1) is a small portable computerized device that delivers rapid-acting insulin via an infusion set which includes a flexible, plastic tube (called a cannula) that is inserted under the skin.
- Insulin pump was first developed with the size of a back-pack in the 1960’s.
- The current form of insulin pump was first used in 1983.
Although the use of insulin pumps in the West has increased by leaps and bounds especially among the type 1 diabetic individuals, its use in Malaysia remains very limited.
Insulin pump was first used in Malaysia in 2001. At present, there are about 100 diabetic individuals on insulin pump therapy in Malaysia.
How Do Insulin Pump Work?
The insulin pump delivers insulin in 2 ways :
1) The basal insulin infusion.
- The basal insulin infusion that replaces the intermediate- or long-acting subcutaneous insulin injection delivers insulin continuously according to the pre-set rates adjusted based on the individual unique requirement throughout the day.
- It is meant to keep blood glucose under control in between meals and during sleep.
- The pump can be programmed to deliver basal insulin at different rates according to the time of the day according to each individual’s unique requirements.
2) The bolus insulin dosing.
The bolus dose that replaces rapid- or short-acting subcutaneous insulin injection covers for the rise in blood glucose in response to meals as well as snacks intake, it is also used to correct for unexpectedly high blood glucose during
- stress,
- intercurrent sickness,
- underestimation of carbohydrate intake etc.
The exact dose of bolus insulin to be delivered can be calculated using the Bolus Wizard® calculator based on a pre-set formula taking into account of an individual sensitivity to insulin, target blood glucose and residual amount of last dose of bolus insulin given (i.e. ‘active’ insulin) at that particular time when the dose is to be delivered.
The mode of bolus delivery can also be administered via 3 different ways, i.e. the standard, dual wave or square wave bolus based on the meal composition (proportion of carbohydrate, protein and fat) as well as the duration of meal consumption.
Insulin pump therapy has the best ability to mimic the insulin release from a healthy functioning pancreas by delivering insulin at a rate and dosing customized to an individual’s needs which is not achievable with the conventional subcutaneous insulin injection (Fig. 2).
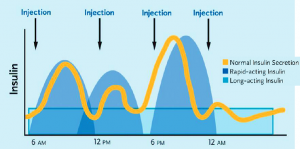 Figure 2(a) : Comparison of insulin action curve of a normal healthy individual with a diabetic patient receiving basal bolus insulin injection showing significant mismatch.
Figure 2(a) : Comparison of insulin action curve of a normal healthy individual with a diabetic patient receiving basal bolus insulin injection showing significant mismatch.
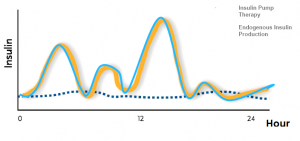 Figure 2(b) : Continous subcutaneous insulin infusion using an insulin pump is the most physiological method of insulin delivery currently available.
Figure 2(b) : Continous subcutaneous insulin infusion using an insulin pump is the most physiological method of insulin delivery currently available.
Who Should Use Insulin Pump?
Insulin Pump therapy should be considered in diabetic individuals of all ages requiring insulin therapy with the following situations :
-
-
- Recurrent episodes of low blood glucose (i.e. hypoglycemia) especially overnight and or induced by physical activities.
- Impaired ability to recognise hypoglycemia (i.e.hypoglycemia unawareness) predisposing an individual to severe hypoglycemic events.
- Dawn phenomenon, i.e. a rise in blood glucose in the morning due to the rise in corresponding cortisol levels in the blood.
- Individuals who are highly sensitive to insulin with extremely low insulin requirement.
- Individuals with high insulin requirement, e.g. more than 1.5u/kg/day.
- Children with unpredictable pattern of food intake and physical activities.
- Woman who are trying to conceive or are already pregnant with suboptimal blood glucose control.
- Shift workers.
- Athletes.
- Delayed carbohydrate absorption after meals due to delayed emptying of the food from the stomach to small intestine (i.e. gastroparesis) resulting in prolonged elevation in blood glucose after meals.
- Recurrent diabetic ketoacidosis.
-
Advantages of Insulin Pump
Some advantages of using an insulin pump instead of subcutaneous insulin injections are :
-
-
- The customised setting of an insulin pump allows significantly greater flexibility in lifestyle in following aspects :
-
- When, what and how frequent you want to eat?
- When and for how long you want to exercise for?
- What time you want to sleep?
-
-
- Reduction of severe hypoglycemic events especially the overnight hypoglycemia in individuals with hypoglycemic unawareness (1).
- Elimination of the need of multiple subcutaneous insulin injections. For example, an individual who is previously on basal bolus insulin regimen will only need to change of insulin infusion set 10 times as opposed to delivering 120 injections in a month.
- Insulin pump allows delivery of insulin dose in a more precise manner as it allows the fine tuning of insulin dose down to as low as 0.05unit per hour for basal infusion and 0.1u for bolus dosing. This is especially important for individuals with high insulin sensitivity or the pediatric population.
- Reduction in large swings in blood glucose levels by eliminating the unpredictable effects of intermediate- or long-acting insulin.
- Easy delivery of bolus insulin for meals, snacks and correction of high blood glucose just by a press of button.
- The improved insulin absorption allows reduction in total daily insulin requirement (2).
- The use of Insulin pump has been associated with significant improvement in HbA1C in both type 1 and type 2 diabetes (3-4) in prospective randomised controlled trials.
- The use of dual wave or square wave bolus feature can address the problems of prolonged elevation in blood glucose after meals in gastroparesis or when the meal has to be consumed over a prolonged period.
- Obviating the need for insulin adjustment when travelling across time zone, only the clock of the insulin pump need s to be reset to the local time.
-
Disadvantages of Insulin Pump
The disadvantages of using an insulin pump include :
-
-
- Significant start-up cost and maintenance cost.
- Need to be attached to the pump almost all the time.
- Need to undergo training for handling of insulin pump.
- May cause diabetic ketoacidosisif the cannula is dislodged unknowingly resulting in interruption of insulin delivery for hours.
-
Getting Started With An Insulin Pump
Once you have decided to commence on insulin pump with your diabetes care team, your doctor will work out the preliminary insulin pump setting including the basal infusion rate, carbohydrate ratio and insulin sensitivity factor based on your pre-pump total daily insulin dose or your body weight. The pump setting will then be further adjusted based on your 8-point finger-prick blood glucose readings at home.
The consumables or accessories required for starting on insulin pump therapy include an auto-insertion device (serter), an infusion set, a reservoir, a glucometer and glucose testing strips (Fig. 3).
Figure 3 : The consumables or accessories required for starting on insulin pump therapy.
Individuals who are being commenced on insulin pump therapy should be committed to the following prerequisites :
-
-
- prepared to take on new knowledge.
- willing to perform finger-prick blood glucose 8 times a day initially during the period of pump setting adjustment and at least 4 times a time subsequently during maintenance.
- willing to perform carbohydrate counting or quantification of carbohydrate intake to ensure optimal dose of bolus insulin can be delivered.
- comply to regular follow-up with the diabetes care team.
-
Upon commencing on insulin pump therapy, you will be given training on the following :
-
-
- handling of insulin pump including inserting insulin into the pump reservoir, change of infusion set, carbohydrate counting, button pushing etc.
- performing finger-prick blood glucose 8 times a day.
- treatment of low or high blood sugar.
- insulin handling during sick days.
-
Maintenance of Insulin Pump
It may take several weeks to get used to the insulin pump. Here are some practical tips recommended during maintenance therapy :
-
-
- The insulin pump may be disconnected temporarily during shower, swimming or contact sports. However, it should not be longer than 1 to 2 hours. You may consider giving yourself a supplemental insulin injection if the reconnection is delayed or your blood glucose is high.
- Although the insulin pump allows more flexibility in the meal selection, it’s important to keep to a healthy diabetic diet that is high in fiber, low in sugar, fat and salt to avoid weight gain and worsening control of your blood cholesterol or blood pressure.
- Record down finger-prick blood glucose readings (4 to 8 times per day) along with carbohydrate estimation , physical activities and correction dose given at least weekly. A detailed review with your diabetes care team will be the key to a successful outcome of you insulin pump therapy.
- When traveling, always bring extra supplies of insulin pump consumables, pump batteries, as well as insulin pen in case you are not able to use the pump for some reason.
-
What Type of Support Service Do I Need While On Pump
-
-
- A diabetes care team which consists of an endocrinologist or a diabetologist; a diabetes nurse educator and a dietitian.
- Technical product support service that is able to provide assistance 24 hours a day.
-
What Does The Future of Insulin Pump Hold?
The latest model of insulin pump can now be incorporated with a real-time continuous glucose monitoring system (CGMS) which provide instant feedback to the pump user on the blood glucose levels. This will allow the user to act on the high or low blood glucose immediately by administering correction bolus or suspend the insulin pump temporarily. A close loop system involving instant feedback of real-time blood glucose back to the pump along with automated control of insulin release or suspension is currently under development.
A pilot study on the use of a ‘bionic pancreas’, a system that uses continuous blood glucose monitoring along with subcutaneous delivery of rapid-acting insulin (to lower blood glucose) and glucagon (to raise blood glucose) directed by a computer algorithm every 5 minutes is recently published. Compared to the conventional insulin pump, the ‘bionic pancreas’ improved blood glucose control with less hypoglycemic events (5).
Conclusion
As the most physiological method of insulin delivery currently available, Insulin pump therapy is a treatment option for people with diabetes that allows more flexibility by matching the insulin delivery with an individual’s lifestyle, more stable insulin absorption, less unpredictable swings in blood glucose thus leading to better quality of life along with better blood glucose control (6-8). With further technological advancement, a completely automated system of insulin delivery that simulate the normal insulin secretion from a healthy pancreas may be available in the near future.
References
-
-
- Parkner T et al. Diabetic Med 2008; 25: 585-91.
- Peyrot M et al. Diabetes Care 2005; 28:53–58.
- Pickup JC et al. Diabet Med 2008; 25: 765-774.
- Reznik Y et al. Lancet 2014. Published online 4 July 2014. http://dx.doi.org/10.1016/S0140-6736(14)61037-0.
- Russell SJ et al. New Eng J Med 2014, 371:313-25.
- The Equality Study Group. Diabetic Med 2008; 25: 213–220.
-
| Last reviewed | : | 17 May 2016 |
| Writer | : | Dr. Foo Siew Hui |
| Accreditor | : | Dr. Zanariah binti Hussein |
 PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia
PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia