Introduction
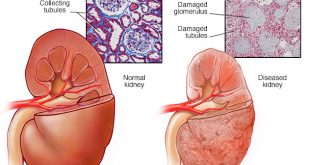
Chronic kidney disease (CKD) affects drug elimination and other processes involved in drug disposition (e.g., absorption, drug distribution and metabolism). Patients with diabetic kidney disease often have multiple medical problems and therefore may be exposed to agents with potential nephrotoxicity (risk of causing damage to the kidneys).
Inappropriate dosing can result in adverse drug reaction or ineffective therapy with poor outcomes.
So what you need to know?
- Get your doctor to review all medications regularly to ensure the dose is appropriate.
- Drugs need to be adjusted based on estimated glomerular filtration rate (GFR) and with declining renal function
- Ask your doctor before you start
-
- any new medication
- buy any over-the-counter medicine
- herbal/traditional medicine
-
Special precautions:
- Avoid Painkillers eg: NSAIDs including COX-2 Inhibitors (such as mefenamic acid diclofenac, ibuprofen, naproxen, indomethacin, ketoprofen, salicylic acid [high dose], meloxicam, celecoxib, and etoricoxib)
- Avoid radio-contrast agents for radiological procedure unless absolutely indicated
- Oral sodium phosphate (FLEET®) in bowel preparation for colonoscopy in CKD stage 4 – 5 (link to CKD classification)
- A blood test for kidney function should be done before, after starting and also after increasing dosage of Angiotensin-Converting Enzyme Inhibitor (ACEi)/Angiotensin Receptor Blocker (ARB). These agents are used in kidney disease for either blood pressure control/ reduction in ‘proteinuria’
- Hypoglycemic agents in kidney failure:
- Long-acting sulphonylureas (chlorpropamide/glibenclamide) should be avoided due to their long biological effect
- Metformin should be avoided if the serum creatinine is above 150 -200umol/L
-
- can rarely cause lactic acidosis in kidney failure
-
- Thiazolidinediones can cause fluid retention
- Insulin: your doctor will usually reduce the dose in kidney failure to avoid hypoglycaemia (low blood sugar level). Insulin is degraded by the kidney
References
- Medscape Reference: Guidelines for Drug Dosing Regimens in Chronic Kidney Disease Am Fam Physician. 2007;75:1487-1496
- Malaysian Clinical Practice Guideline: Management of Chronic Kidney Disease in Adult 2011
- Malaysian Clinical Practice Guideline: Diabetic Nephropathy July 2004
| Last Reviewed | : | 6 June 2016 |
| Writer | : | Dr. Shahnaz Shah Firdaus Khan |
| Accreditor | : | Dr. Sunita Bavanandan |
 PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia
PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia