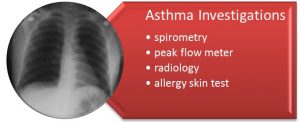
To diagnose asthma and distinguish it from other lung disorders, doctors rely on a combination of medical history, physical examination, and laboratory tests, which may include:
- Spirometry
A spirometer is a device used by your child’s physician that assesses lung function when the child come for asthma review in the clinic. This test is used in children older than 5 years. The spirometer has two pieces: a mouthpiece and a tube that connects to a machine, which records and displays the results. Spirometry, the evaluation of lung function with a spirometer, is one of the simplest, most common pulmonary function tests and may be necessary for any/all of the following reasons:- To determine how well the lungs receive, hold, and utilize air
- To monitor a lung disease
- To monitor the effectiveness of treatment
- To determine the severity of a lung disease
- To determine whether the lung disease is restrictive (decreased airflow) or obstructive (disruption of airflow)
Spirometry is useful in the clinic setting during asthma follow up. The result of the child’s lung function will be determined immediately during the clinic review.
Watch video: Link to http://www.youtube.com/watch?v=YHKHIR7KenU

Source: http://www.seattlechildrens.org/content.aspx?id=5238
- Peak flow meter (PFM)
A device used to measure the amount of air a person can blow out of the lungs. During asthma or other respiratory flare up, the large airways in the lungs slowly begin to narrow. This will slow the speed of air leaving the lungs and can be measured by a PFM. This measurement is very important in evaluating how well or how poorly the disease is being controlled.
In an outpatient setting, measurement of the peak flow rate by using a peak flow meter can provide useful information about obstruction in the large airways. Take care to ensure maximum patient effort. However, a normal peak flow rate does not necessarily mean a lack of airway obstruction.
Even in the inpatient setting, measurement of the peak flow rate will give us the progress of the child’s airway status. It is usually been done in older kids who can perform the PFM.
Watch Video: http://www.youtube.com/watch?v=6oKupWgDu80
 Peak Flow Meter
Peak Flow Meter - Radiology
- Radiography and CT Scan
Include chest radiography in the initial workup if the asthma does not respond to therapy as expected. In addition to typical findings of hyperinflation and increased bronchial markings, a chest radiograph may reveal evidence of parenchymal disease, atelectasis, pneumonia, congenital anomaly, or a foreign body.
In a patient with an acute asthmatic episode that responds poorly to therapy, a chest radiograph helps in the diagnosis of complications such as pneumothorax or pneumomediastinum. Consider using sinus radiography and CT scanning to rule out sinusitis.
- Radiography and CT Scan
- Allergy Tests
Allergy testing can be used to identify allergic factors that may significantly contribute to the asthma. Once identified, environmental factors (eg, dust mites, cockroaches, molds, animal dander) and outdoor factors (eg, pollen, grass, trees, molds) may be controlled or avoided to reduce asthmatic symptoms.
Allergens for skin testing are selected on the basis of suspected or known allergens identified from a detailed environmental history. Antihistamines can suppress the skin test results and should be discontinued for an appropriate period (according to the particular agent’s duration of action) before allergy testing. Topical or systemic corticosteroids do not affect the skin reaction.

Reference:
- Ministry Of Health Malaysia. Clinical Practise Guideline For Management Of Childhood Asthma 2014.
- Global Strategy for Asthma Management and Prevention: Global Initiative for Asthma (GINA) (updated 2012).
- Link to http://www.youtube.com/watch?v=6oKupWgDu80
- Link to http://www.youtube.com/watch?v=YHKHIR7KenU
| Last Reviewed | : | 5 November 2015 |
| Writer | : | Dr. Noor Hafiza bt. Noordin |
| Accreditor | : | Dr. Norzila bt. Mohamed Zainudin |
 PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia
PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia