Introduction
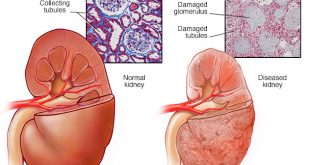
Iron is essential for the formation of red blood cell haemoglobin. Iron deficiency is common in patients with chronic kidney disease. This is especially true of patients on haemodialysis for the most advanced level of kidney impairment known as CKD stage 5 patients on haemodialysis where it has been shown that among patients receiving ESAs (erythropoiesis-stimulating agents), more than 50% are iron deficient5.
Even if a CKD patient is not iron deficient when starting ESA therapy, the ESA therapy will stimulate new red blood cell formation and patient’s iron stores may become depleted by the addition of iron into new haemoglobin molecules. Therefore, most patients receiving ESAs will require simultaneous iron therapy.
Tests for iron status
The aim of evaluating iron status is to assess:
- Iron levels in tissue stores and
- The availability of iron to be used for production of new red blood cells
Serum ferritin level is the only available blood marker of storage iron. Ferritin is a protein in the body that binds to iron. Most of the iron stored in the body is bound to ferritin. Ferritin levels < 100 µg/mL indicate an absolute iron deficiency. High ferritin levels, however, may not always indicate adequate iron stores as the serum ferritin levels can increase in infection, inflammatory states or in liver disease. The lower level of ferritin should be 100 ng/ml in CKD patients not yet on dialysis or those treated with peritoneal dialysis 1. For patients on haemodialysis, the lower level advised for ferritin is 200 ng/ml. Target levels recommended are 200-500 ng/ml 1.
There are several tests to assess the availability of iron for use. These include transferrin saturation (TSAT), the percentage of hypochromic red blood cells and reticulocyte content. TSAT is the most commonly used test because the last two tests are not widely available. Transferrin is a protein produced by the liver. It serves to bind iron and carry it in the bloodstream to the bone marrow. Transferrin saturation is a calculated value based on blood tests to measure the amount of iron bound to transferrin in the blood. The lower limit advised for TSAT is 20% and recommended target levels are 30-50% 1. Limitations of TSAT as a test include day to day variations and the fact that it is influenced by nutritional status and inflammation.
It is important to take and interpret the tests for anaemia and iron status together. The combination of tests provides important information on red blood cell production (haemoglobin level), iron stores (ferritin) and iron availability to the bone marrow (TSAT). Test results should also be interpreted with caution because of the limitations as outlined above.
If the ferritin is adequate but TSAT is low (i.e < 20%) the patient is deemed to have a “functional iron deficiency”. This means there is an imbalance between the iron requirements of the bone marrow and the actual iron supply. In this situation, the patient would need iron supplementation.
Causes of iron deficiency
In CKD patients, a number of irregularities in the way the body handle iron can lead to iron-deficiency. This include:
- Inadequate oral iron intake
- low protein diets
- poor appetite
- Inadequate iron absorption
- Antacid therapy or higher pH (acid-alkali status) in the stomach
- Phosphate binding therapy (e.g. calcium carbonate)
- Competition from other metals (e.g. copper, lead)
- Increased blood loss
- Dialysis blood loss e.g. blood remaining in the dialysis tubing and dialyzer at the end of each dialysis session
- Blood loss from the stomach and/or intestines due to
- High levels of waste products in the blood causing bleeding problems
- Use of medications that thin the blood
- Use of medications that may induce inflammation or ulceration on the stomach lining
- Frequent blood tests
- Abnormal iron utilisation4
- Accelerated formation of new red blood cells due to ESA therapy
- Decreased iron storage due to longstanding inflammation or infection
- Decreased transferrin due to malnutrition or chronic disease
- Impaired release of iron stores due to inflammation
Management of iron deficiency
The first step in the management of iron deficiency is to look for causes and to correct these as much as possible. The next step is to provide iron supplements. These are available in oral and intravenous forms.
In most patients with CKD who are not yet on dialysis or on peritoneal dialysis, oral iron supplementation is sufficient and should be the first line of treatment. However, some patients may not be able to tolerate oral iron because of side effects or oral iron may be ineffective in maintaining adequate body stores of iron. In such cases, an intravenous iron administration may be required.
Side effects of oral iron include nausea, stomach discomfort, black stools, diarrhoea or constipation. Various oral iron preparations are available (see table 1) and the frequency of side effects is dependent on the amount of elemental iron contained. For patients who have difficulty tolerating oral iron supplements, the following measures may be helpful:
- Using smaller, more frequent doses
- Starting with a lower dose and increasing slowly to the target dose
- Trying a different oral iron product
- Taking the supplement at bedtime.
Tips to increase absorption of oral iron supplements:
- Take oral iron on an empty stomach – when food is eaten within 2 hours before or 1 hour after an oral iron supplement, the food will reduce iron absorption by as much as one-half. 2
- Avoid taking phosphate binders ( e.g. calcium carbonate) with oral iron supplements as these will also reduce oral iron absorption – oral iron should be taken 2 hours before or 1 hour after phosphate binders 3
Table 1. Oral iron preparations available in Malaysia and their elemental iron content
| Iron salt | Dose | Elemental iron content (ferrous iron content) |
| Ferrous fumarate | 200 mg | 65 mg |
| Ferrous sulphate | 300 mg | 60 mg |
| Ferrous sulphate dried | 200 mg | 65 mg |
| Ferrous gluconate | 300 mg | 35 mg |
The drawbacks of intravenous iron are that it costs more and its safety profile is less clear compared to oral iron. There are concerns regarding rare but serious allergic reactions and the possibility of increased infections. Various intravenous preparations available in Malaysia – iron dextran, low-molecular-weight iron dextran (Cosmofer®) and iron sucrose complex (Venofer®).
References:
- Locatelli F, Adrian Covic A, Eckardt K -U, Wiecek A and Vanholder R on behalf of the ERA-EDTA ERBP Advisory Board. (2009) Anaemia management in patients with chronic kidney disease: a position statement by the Anaemia Working Group of European Renal Best Practice (ERBP) Nephrol Dial Transplant 24: 348–354
- Piraio-Biroli G, Bothwell TH, Finch CA. (1958) Iron absorption. II. The absorption of radioiron administered with a standard meal in man. J Lab Clin Med 51:24-36
- Post Graduate Renal Society Malaysia (2009). Renal Replacement Therapy Clinical Practice Guidelines 3rd Edition Kuala Lumpur. ISBN: 978-983-44908-0-5
- Silverberg DS, Wexler D, Iaina A and Schwartz D. (2011). Correction of Iron Deficiency in the Cardiorenal Syndrome. International Journal of Nephrology Article ID 365301, 8 pages doi:10.4061/2011/365301
- US Renal Data System: The USRDS Dialysis Morbidity and Mortality Study (Wave 1) in National Institutes of Health, National Institute Diabetes and Digestive and Kidney Diseases (eds): US Renal Data System 1996 Annual Data Report. Bethesda, MD, 1996 www.usrds.org/download/1996begin.pdf
| Last Reviewed | : | 12 May 2016 |
| Writer | : | Dr. Sunita Bavanandan |
| Accreditor | : | Dr. Hooi Lai Seong |
 PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia
PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia