Introduction
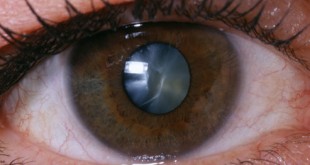
Diabetes can cause a variety of eye problems, the most common being diabetic retinopathy. Diabetic retinopathy is defined as retinopathy (damage to the retina) caused by microvascular complications of diabetes. Other conditions associated with diabetes and the eye include cataracts, cornea abrasion, cornea ulcer, dry eyes,,glaucoma and ocular motor nerve palsies.3
In Malaysia, diabetic eye disease is the commonest cause of visual loss among adults of working age. Prevalence of Diabetic Retinopathy is closely linked to the duration of Diabetes mellitus. At diagnosis, less than 5% will have retinopathy while the prevalence rises to 40 – 50% after 10 years. In Malaysia, the prevalence of Diabetic Retinopathy from the 2007 Diabetic Eye Registry was 36.8%.2
Symptoms
Diabetic retinopathy usually affects both eyes. It is uncommon to have symptoms in the early stages of diabetic retinopathy. However, as the condition progresses, the symptoms may include : 4
- Blurred vision – sudden or gradual
- Pain in the eye
- Seeing spots
- Loss of vision
- Double vision
- Floaters in your vision
Complications of retinopathy in later stages can include blindness or retinal detachment. Hence, if you are diabetic, please have your eye check at least once a year or if you experience any of the symptoms.
Assessment of Diabetic Retinopathy (DR)
The initial assessment should be conducted at the time of diagnosis of type 2 diabetes mellitus (T2DM) and annually if there is no retinopathy.
Pregnant women with T2DM (not gestational diabetes) should have retinal examination during each trimester. 1
A variety of screening modalities are available in detecting and classifying DR. Non-mydriatic fundus camera should be used as a screening tool for diabetic retinopathy (DR) when possible.(Grade A)
When there is no access to fundus camera, ophthalmoscope should be used for screening of DR. Fundus examination must be conducted through a dilated pupil (tropicamide 0.5% or 1.0%) by using a direct ophthalmoscope to improve sensitivity. The ultimate aim for screening of DR is to detect sight threatening DR and to ensure timely treatment in order to prevent vision loss. 2
Diabetic Retinopathy Grading2
Table 1 : International Clinical Diabetic Retinopathy and Diabetic Macula Oedema Disease Severity Scale
| RETINOPATHY STAGES | FINDINGS ON OPHTHALMOSCOPY |
| No apparent retinopathy
|
No abnormalities |
| Mild non-proliferative DR
(NPDR) |
Microaneurysms only
|
| Moderate NPDR
|
More than just microaneurysms but less than severe NPDR
|
| Severe NPDR
|
Any of the following:
1. More than 20 intraretinal haemorrhages in each of 4 quadrants 2. Definite venous beading in 2 or more quadrants 3. Prominent intraretinal microvascular abnormalities in 1 or more quadrants AND no signs of proliferative retinopathy
|
| Proliferative DR (PDR)
|
One of the following:
1. Neovascularisation 2. Vitreous/preretinal haemorrhage
|
| Advanced Diabetic Eye Disease
(ADED)
|
One of the following:
1. Formation of fibrovascular tissue proliferation 2. Traction retinal detachment due to formation of posterior vitreous detachment 3. Dragging of retinal/distortion 4. Rhegmatogenous retinal detachmentings on Ophthalmoscopy |
| MACULA OEDEMA | FINDINGS ON OPHTHALMOSCOPY |
| Absent | No retinal thickening or hard exudates in posterior pole
|
| Present
|
• Mild – some retinal thickening or hard exudates in posterior pole but distant from the macula
• Moderate – retinal thickening or hard exudates approaching the centre of the macula but not involving the centre • Severe – retinal thickening or hard exudates involving the centre of the macula
|
Recommendation
Achieve and maintain tight glycaemic and blood pressure control.
Criteria for Urgent Referral 2
| Urgency of referral | Ocular features |
| Emergency (same day referral)
|
• Sudden severe visual loss
• Symptoms or signs of acute retinal detachment |
| Within 1 week
|
• Presence of retinal new vessels
• Preretinal haemorrhage • Vitreous haemorrhage • Rubeosis iridis
|
| Within 4 weeks
|
• Unexplained drop in visual acuity
• Any form of maculopathy • Severe NPDR • Worsening retinopathy |
References
- Ministry of Health. Clinical Practive Guideline Management of Type 2 diabetes. 2009
- Ministry of Health. Clinical Practice Guideline Screening of Diabetic Retinopathy. 2011
- EAM Gale, JV Anderson. Diabetes mellitus and other disorders of metabolism. Kumar and Clark Clinical Medicine 2002 : 1093–1095.
Top of Form
Bottom of F4. Diabetic retinopathy symptoms.www.diabetes.co.uk.
QUIZ
- Diabetic eye disease is the most common cause of visual loss among adults?
- Yes
- No
- Not sure
Answer: yes
- Complications of diabetic retinopathy include retinal detachment?
- Yes
- No
- Not sure
Answer: yes
- Pregnant women with Type 2 Diabetes mellitus should have retinal examination during each trimester?
- Yes
- No
- Not sure
Answer: yes
 PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia
PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia