Chronic Complication – Macrovascular
Peripheral Vascular Disease (PVD) in Diabetics
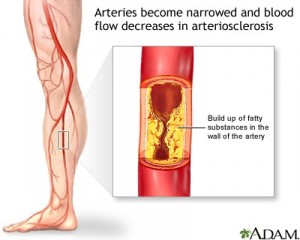
Peripheral vascular disease is one of the common complications of poorly controlled diabetes. It refers to disease of circulatory system especially in lower limbs of diabetes. It occurs 20 times more common among diabetics than non diabetics. Persistent high level of glucose in the blood circulation of diabetics can damage the vessels and it becomes either narrowed or weakened. Most diabetics also have high blood pressure and high cholesterol in the blood, which accelerates the development of atherosclerosis, a build-up of fatty material within the vessels.
Other risk factors for developing peripheral vascular disease are
- past and family history of premature heart attacks or strokes
- older people
- overweight or obesity
- inactive (sedentary) lifestyle
- smoking – is a very strong risk factor for developing peripheral vascular disease
What are the symptoms of Peripheral Vascular Disease?
About half of people with peripheral vascular disease do not have symptoms. Symptoms are usually caused by the leg muscles not getting enough blood. It depends partly on which artery is affected and to what extent blood flow is restricted. The most common symptom of peripheral vascular disease called intermittent claudication. It is :
- leg pain upon activity and relieved by rest
- usually a dull, cramping pain or heaviness, tightness, or tiredness in the muscles
- pain at night may indicate complete blocked
- If symptoms persist even while at rest is a sign of more severe disease.
Other symptoms :
- Numbness and tingling sensation,
- weakness in the legs,
- burning or aching pain in the feet or toes while resting,
- a sore on a leg or a foot that will not heal,
- one or both legs or feet feel cold or change color (pale, bluish, dark reddish),
- loss of hair on the legs
- Impotence.
When to seek medical help?
If you have any of above symptoms you should seek medical assessment and treatment early. All diabetics especially those with other co-risk factors should have regular lower limbs assessment.
Assessment
These aim to measure the severity of the pain and how its affect your quality of life. It is also very important to determine the possible causes, associated risk factors and complications.
Treatment
Treatment depends on the underlying cause of your disease, the severity of your condition, and your overall health.
Medications
- Medications used that aim to lower the risk and progression of atherosclerosis throughout the body, such as those to help stop smoking, lower blood pressure, lower cholesterol, and optimize the blood sugar control.
- Medications for direct treatment of the symptom of intermittent claudication.
- Pentoxifylline (Trental) : This drug helps to improve blood flow by decreasing the viscosity of blood and making red blood cells more flexible.
- Antiplatelet agents include aspirin, ticlopidine, and clopidogrel prevent further clots from forming by preventing blood cells and platelets from clumping together.
- Anticoagulant agents include heparin, warfarin(Coumadin), and low-molecular-weight heparin: These agents interfere with the sequence of blood clotting factors that causes a clot to form.
- Thrombolytics: These are powerful drugs that can actually dissolve an existing clot. They can be used only under certain circumstances and are given only in the hospital.
Self-Care at Home
Modifying risk factors for atherosclerosis and peripheral vascular disease can not only prevent disease from getting worse but can also actually reverse the symptoms.
- Follow your health care provider’s recommendations in controlling your blood sugar, blood pressure and high cholesterol.
- Footcare – Fitting shoes, keep feet dry and clean, special attention while trimming your own toenails and avoid injuries to prevent skin breakdown, gangrene, and loss of toes.
- Quit smoking: Quitting smoking reduces symptoms and lowers the chance of having peripheral vascular disease get worse.
- Get active: Regular exercise, such as walking, can reduce symptoms and increase the distance you can walk without symptoms.
- Eat nutritious, low-fat foods and avoid foods high in cholesterol.
- Maintain a healthy weight.
- Avoid certain cold medications. Over-the-counter cold remedies that contain pseudoephedrine constrict your blood vessels and may increase the symptoms
- It may be helpful to raise the head of your bed by four to six inches (10 to 15 centimeters), because keeping your legs below the level of your heart usually lessens pain.
- Avoid cold temperatures as much as possible.
No strong evidence that circulation of the vessels affected by peripheral vascular disease would be restored by massage.
Interventional procedures
Depending on your symptoms, your doctor may suggest angioplasty, a technique to enlarge a blocked or narrowed artery without surgery. Some patients may need surgery or a bypass.
Follow-up
Follow the recommendations of your health care provider for risk factor reduction. If he or she recommends medication, take the medication as directed. Report changes in your symptoms and any side effects you experience.
Complications
If untreated, Peripheral vascular disease can develop complications :
- Permanent numbness, tingling, or weakness in legs or feet
- Permanent burning or aching pain in legs or feet
- Gangrene: This is a very serious condition. It is the result of a leg or foot or other body part not getting enough blood. The tissues die and begin to decay. The only treatment is amputation of the affected body part.
- People with PVD are at higher risk of heart attack and stroke.
Prevention
The best way to prevent Peripheral vascular disease is to reduce your risk factors.
- Control your blood sugar level and take care of your feet. Ask your doctor what your HbA1C is, a measure of how well your blood sugar is controlled. If it is not controlled, and your risk of peripheral vascular disease escalates.
- Do not smoke. Quitting smoking can reduce the symptoms of peripheral vascular disease and prevent disease progression.
- Eat nutritious, low-fat foods; avoid foods high in cholesterol.
- Maintain a healthy weight.
- Engage in moderately strenuous physical activity for at least 30 minutes a day. At least walk briskly for 20-30 minutes daily.
- Control high blood pressure and reduce high cholesterol.
References
- Malaysian CPG on Management of Type 2 Diabetes Mellitus(4th Edition), 2009
- Clinical Guidelines for Type 2 Diabetes : Prevention and Management of Foot Problems. NICE Clinical Guidelines, No. 10.
- Watson L, Ellis B, Leng GC. Exercise for intermittent claudication.Cochrane Database Syst Rev. 2008. Issue 4. Art No.: CD000990. DOI: 10.1002/14651858.CD000990.pub2.
- Mills JL. Lower extremity arterial disease. In: Cronenwett JL, Johnston W, eds.Rutherford’s Vascular Surgery. 7th ed. Philadelphia, Pa: Saunders Elsevier; 2010:section 15.
 PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia
PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia