Introduction
Foot examination is part of an integral management of diabetes. Foot problems may develop after more than 10 years of diabetes duration.
Diabetes foot ulcers develop secondary to chronic ischaemia (insufficient blood supply to the foot) due to microvascular (small vessels) and macrovascular (large vessels) complications of diabetes (5]. Apart from these, diabetes neuropathy (abnormal function of the nerves) also plays a role in the development of foot ulcers [5].
Diabetes foot complications are the most common non traumatic lower extremity amputations in the industrialized world.
Moreover it is the most frequent reason for hospitalization in patients with diabetes. It accounts for up to 25% of all diabetic admissions in the USA and Great Britain [2, 3, and 4].
Why to Do Foot Examination?
Diabetes patients must do regular foot examination. Poor circulation and neuropathic sequelae of a diabetes foot can turn minor breakdowns into severe ulceration.
About 15 percent of people with diabetes will develop foot ulceration. Half of these ulcerations will later lead to amputation [1].
Foot examination is intended to detect early changes and high risk foot. Once detected the foot has to be managed accordingly. Patient and family members should be educated on foot care.
Proper foot care can delay complications and amputation.
How Often Should Foot Examination Be Done?
Foot examination should be done annually. However more frequent examination is needed if the foot is at high risk of getting ulcers.
What Are the Elements Tests in Foot Examination?
Foot examination must include assessment of :
- Neurological status
Neurological status can be checked using 10 gram monofilaments to determine whether the patient has “protective sensation”
A 128 C tuning fork is used to determine presence of vibratory sensation at the ankle and first metatarsal-phalangeal joints
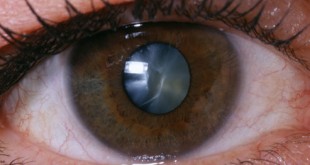
- Vascular status
Vascular assessment is important to determine the competency of peripheral circulation. It is also used to assess eventual ulcer healing and essential in the evaluation of diabetic ulcers.
Assessment includes checking for dorsalis pedis pulse on the dorsum of the foot and the posterior tibial pulse behind the medial malleolus.
Capillary returns are also assessed and should not be more than 2 seconds.
Ankle brachial index using a Doppler is also a useful tool in vascular assessment.
- Ulcer evaluation
Ulcer evaluation must include comprehensive documentation of the wound’s location, size, shape, depth, base and border. X-rays and magnetic resonance imaging are useful in determining osteomyelitis (infection of the bone) and deep abscesses.
Signs of infection, presence of cellulitis, odor or purulent drainage should be documented.
The pictures below show how a foot is being examined.
Foot examination [1]
Who Does the Foot Examination?
Health care providers should be competent to do foot examination in diabetes patients. Patient and carers must be empowered to do foot examination to detect early changes too.
Risk Factors for Foot Ulcers
- Diabetic neuropathy
- Structural foot deformity
- Peripheral arterial occlusive disease
- Improper foot wear and care
- Visual impairment
- Smoking
- Diabetes nephropathy – abnormal function of the kidneys (especially on haemodialysis)
How to Prevent Foot Complications?
- Optimal glucose control
- Optimal treatment of dyslipidaemia (abnormalities in cholesterol and fat profile)
- Treating blood pressure to target
- Proper foot wear and care
- Regular foot examination
Conclusion
Foot examination is essential to ensure amputation is avoided. Diabetes foot ulcers are preventable and must be managed accordingly
References
- http://sydney.edu.au/medicine/diabetes/foot/Fexam1.html– accessed 20th September 2012 (pictures)
- Gibbons G, Eliopoulos GM. Infection of the diabetic foot. In: Kozak GP, et al., eds. Management of diabetic foot problems. Philadelphia: Saunders; 1984:97–102.
- Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation. Basis for prevention. Diabetes Care. 1990; 13:513–21.
- Reiber GE, Pecoraro RE, Koepsell TD. Risk factors for amputation in patients with diabetes mellitus. A case-control study. Ann Intern Med. 1992; 117:97–105.
- Wu, S. C.; Driver, V. R.; Wrobel, J. S.; Armstrong, D. G. “Foot ulcers in the diabetic patient, prevention and treatment”. Vascular health and risk management 2007; 3 (1): 65–76.
 PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia
PENDIDIKAN PESAKIT Kementerian Kesihatan Malaysia